AI tool that predicts side-effect risk in breast cancer patients to be trialled
Artificial intelligence (AI) could help predict if someone with breast cancer is at risk of side effects from surgery or radiotherapy, according to researchers.
It is hoped the technology, which is set to be trialled in the coming years, will allow doctors to provide more individualised care to their patients.
Side-effects of treatment can include scarring, skin changes, heart damage from radiation and lymphoedema, a painful swelling of the arm, according to Dr Tim Rattay, a consultant breast surgeon and associate professor at the Leicester Cancer Research Centre at the University of Leicester.
“Thankfully, long-term survival rates from breast cancer continue to increase, but for some patients, this means having to live with the side effects of their treatment,” he added.
“That’s why we are developing an AI tool to inform doctors and patients about the risk of chronic arm swelling after surgery and radiotherapy for breast cancer.
“We hope this will assist doctors and patients in choosing options for radiation treatment and reduce side effects for all patients.”
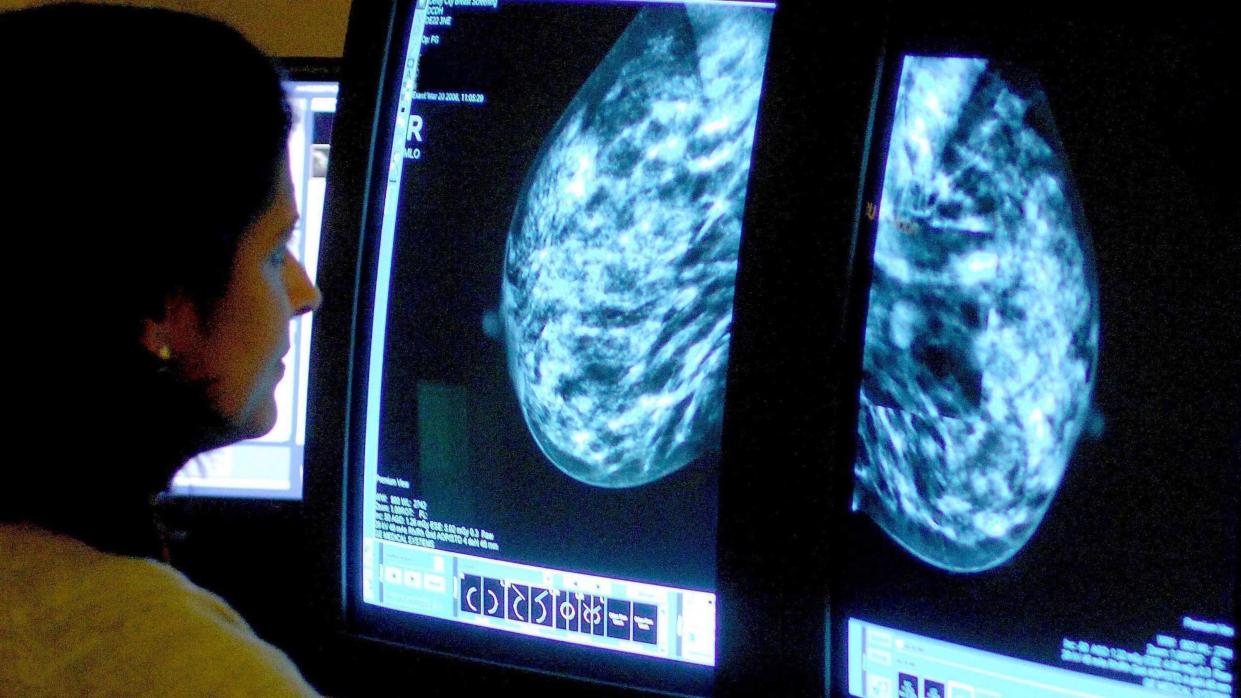
AI is being trialled in some parts of the NHS to help clinicians asses mammograms, which could potentially speed up breast cancer diagnosis.
However, using it to assess the risk of side-effects could lead to more accurate predictions for patients on a personal level.
The technology was trained by researchers to predict arm swelling up to three years after surgery and radiotherapy using data from 6,361 breast cancer patients.
Using AI in this way means patients at a higher risk of arm swelling could be offered additional support, such as wearing an arm compression sleeve during treatment.
Dr Guido Bologna, associate professor at the University of Applied Sciences and Arts of Western Switzerland in Geneva – and co-investigator on the project, said: “The final, best-performing model makes predictions using 32 different patient and treatment features, including whether or not patients had chemotherapy, whether sentinel lymph node biopsy under the armpit was carried out, and the type of radiotherapy given.”
Speaking at the European Breast Cancer Conference in Milan, Dr Rattay said the technology “is an explainable AI tool, which means that it shows the reasoning behind its decision-making”.
“This makes it easier not only for doctors to make decisions, but also to provide data-backed explanations to their patients,” he added.
The current AI model will be incorporated into software that can provide evaluations for doctors and patients and will be tested as part of a clinical trial, known as the PRE-ACT project, which will start recruiting patients from the UK, France and the Netherlands at the end of the year.
The research team hopes to enrol 780 people by early 2026, who will be followed up for a period of two years.
They are also developing the technology further to predict other side effects, including skin and heart damage.
Dr Simon Vincent, director of research, support and influencing at Breast Cancer Now, said: “With over 55,000 people being diagnosed with breast cancer every year in the UK, research looking at how we can improve treatments is urgently needed.
“This exciting project will explore whether using AI could enable people with breast cancer to receive more personalised care and support that helps minimise side effects, such as chronic arm swelling (lymphoedema), after surgery and radiotherapy.
“This research is in its early stages and more evidence is needed before we can consider whether or not the AI tool could be used in medical settings, and we look forward to seeing results from the trial.”


